Uploaded by
genetikdoktoru
COL7A1 Mutations & MMP1 SNP in Dystrophic Epidermolysis Bullosa
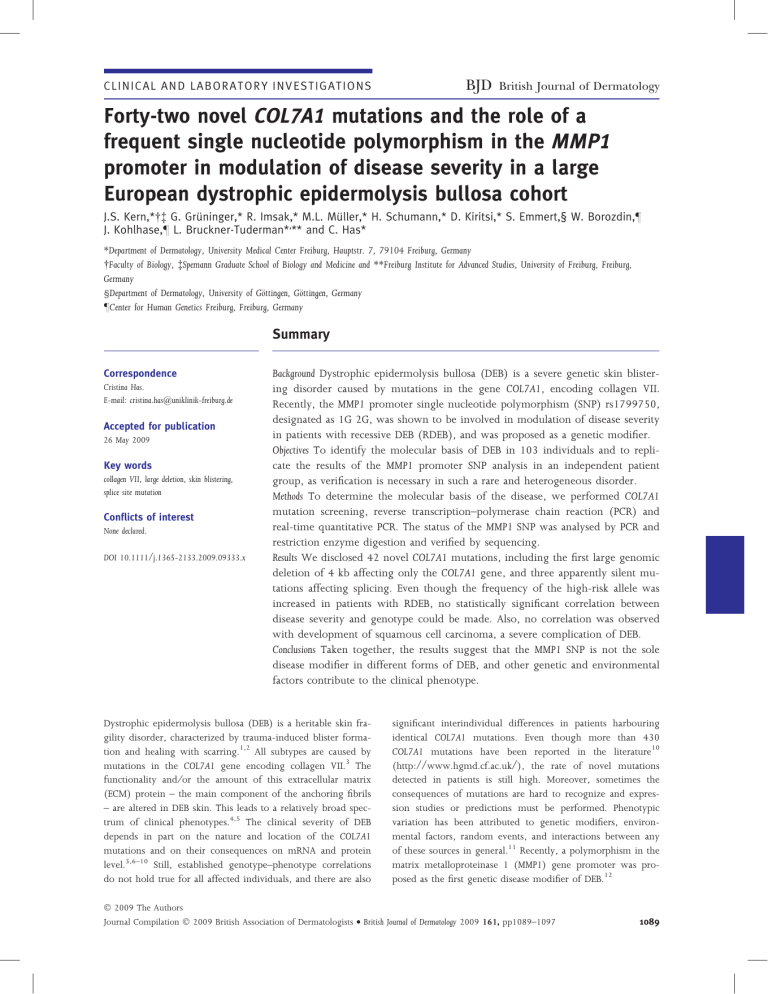
C L I N I C A L A N D LA B O R A T O R Y I N V E S T I G A T I O N S BJD British Journal of Dermatology Forty-two novel COL7A1 mutations and the role of a frequent single nucleotide polymorphism in the MMP1 promoter in modulation of disease severity in a large European dystrophic epidermolysis bullosa cohort J.S. Kern,* G. Grüninger,* R. Imsak,* M.L. Müller,* H. Schumann,* D. Kiritsi,* S. Emmert,§ W. Borozdin,– J. Kohlhase,– L. Bruckner-Tuderman*,** and C. Has* *Department of Dermatology, University Medical Center Freiburg, Hauptstr. 7, 79104 Freiburg, Germany Faculty of Biology, Spemann Graduate School of Biology and Medicine and **Freiburg Institute for Advanced Studies, University of Freiburg, Freiburg, Germany §Department of Dermatology, University of Göttingen, Göttingen, Germany –Center for Human Genetics Freiburg, Freiburg, Germany Summary Correspondence Cristina Has. E-mail: cristina.has@uniklinik-freiburg.de Accepted for publication 26 May 2009 Key words collagen VII, large deletion, skin blistering, splice site mutation Conflicts of interest None declared. DOI 10.1111/j.1365-2133.2009.09333.x Background Dystrophic epidermolysis bullosa (DEB) is a severe genetic skin blistering disorder caused by mutations in the gene COL7A1, encoding collagen VII. Recently, the MMP1 promoter single nucleotide polymorphism (SNP) rs1799750, designated as 1G 2G, was shown to be involved in modulation of disease severity in patients with recessive DEB (RDEB), and was proposed as a genetic modifier. Objectives To identify the molecular basis of DEB in 103 individuals and to replicate the results of the MMP1 promoter SNP analysis in an independent patient group, as verification is necessary in such a rare and heterogeneous disorder. Methods To determine the molecular basis of the disease, we performed COL7A1 mutation screening, reverse transcription–polymerase chain reaction (PCR) and real-time quantitative PCR. The status of the MMP1 SNP was analysed by PCR and restriction enzyme digestion and verified by sequencing. Results We disclosed 42 novel COL7A1 mutations, including the first large genomic deletion of 4 kb affecting only the COL7A1 gene, and three apparently silent mutations affecting splicing. Even though the frequency of the high-risk allele was increased in patients with RDEB, no statistically significant correlation between disease severity and genotype could be made. Also, no correlation was observed with development of squamous cell carcinoma, a severe complication of DEB. Conclusions Taken together, the results suggest that the MMP1 SNP is not the sole disease modifier in different forms of DEB, and other genetic and environmental factors contribute to the clinical phenotype. Dystrophic epidermolysis bullosa (DEB) is a heritable skin fragility disorder, characterized by trauma-induced blister formation and healing with scarring.1,2 All subtypes are caused by mutations in the COL7A1 gene encoding collagen VII.3 The functionality and ⁄or the amount of this extracellular matrix (ECM) protein – the main component of the anchoring fibrils – are altered in DEB skin. This leads to a relatively broad spectrum of clinical phenotypes.4,5 The clinical severity of DEB depends in part on the nature and location of the COL7A1 mutations and on their consequences on mRNA and protein level.3,6–10 Still, established genotype–phenotype correlations do not hold true for all affected individuals, and there are also significant interindividual differences in patients harbouring identical COL7A1 mutations. Even though more than 430 COL7A1 mutations have been reported in the literature10 (http://www.hgmd.cf.ac.uk/), the rate of novel mutations detected in patients is still high. Moreover, sometimes the consequences of mutations are hard to recognize and expression studies or predictions must be performed. Phenotypic variation has been attributed to genetic modifiers, environmental factors, random events, and interactions between any of these sources in general.11 Recently, a polymorphism in the matrix metalloproteinase 1 (MMP1) gene promoter was proposed as the first genetic disease modifier of DEB.12 2009 The Authors Journal Compilation 2009 British Association of Dermatologists • British Journal of Dermatology 2009 161, pp1089–1097 1089 1090 Dystrophic epidermolysis bullosa and MMP1, J.S. Kern et al. MMP1 is a major proteinase of the matrix metalloproteinase (MMP) family that degrades several ECM components, specifically type I collagen and other fibrillar collagens, including collagen VII.13 The involvement of MMP1 in the pathology of DEB has been suspected for a long time.14,15 Increased activity of MMP1, MMP2, MMP3 and MMP9 and decreased tissue inhibitor of metalloproteinase (TIMP)-1 have been detected in the skin of patients more severely affected with DEB. Therefore, it was predicted that phenotypic variability in DEB could be related to interindividual differences in MMP, specifically MMP1, activity.16 The expression level of MMPs in intact skin is very low, but is enhanced under pathological and regenerative conditions, such as inflammation, tumours, wound healing and tissue remodelling. The activity is regulated at three levels: (i) by transcriptional control of MMP genes; (ii) by proteolytic activation; and (iii) by small biological tissue inhibitors (TIMPs).17 The frequent functional single nucleotide polymorphism (SNP) in the MMP1 promoter, )1607del ⁄insG (rs1799750, designated as 1G 2G), modulates the transcription of the MMP1 gene, as the 2G allele forms a recognition site for Ets transcription factor.18 In a French cohort comprising 31 patients with DEB, two genotypes, homozygous 2G (2G ⁄2G) and heterozygous (1G ⁄2G), were associated with a more severe recessive DEB (RDEB) phenotype.12 Almaani et al.19 did not find evidence for the involvement of this SNP in DEB pruriginosa in a group of 27 patients. Instead, they found a possible association of the 2G allele with early-onset squamous cell carcinoma in six individuals with RDEB. As this putative disease modifier could have an important prognostic value and implications for the design of molecular therapy approaches, we assessed its role in a large cohort of European patients with DEB. Materials and methods Patients and clinical samples One hundred and three patients with clinically and morphologically diagnosed DEB were investigated. All patients had caucasian heritage and originated mainly from Central Europe. Following informed consent, ethylenediamine tetraacetic acid (EDTA)-blood and skin samples were obtained. EDTA-blood samples from 40 individuals originating from Central Europe were obtained and used as a control group. The study was approved by the ethics committee of the University of Freiburg. COL7A1 mutation detection Genomic DNA from index patients and parents was extracted from EDTA-blood using the QiaAmp DNA mini kit (Qiagen, Hilden, Germany). Amplification of all 118 COL7A1 exons and exon ⁄intron boundaries and sequencing were performed as previously described.9 Mutations were confirmed by resequencing. For identification of the breakpoints of the COL7A1 genomic deletion the following primers were used for polymerase chain reaction (PCR) and sequencing: F 5¢-TACCTCCAGCGCTCTCCTTC-3¢ and R 5¢-TGGAGAAACACATCAGGGTG-3¢. The mutation c.5499C>T was verified in 100 control chromosomes by restriction endonuclease digestion with MwoI according to the manufacturer’s protocol. The mutation c.6217)3C>A was verified in 150 control chromosomes by direct sequencing. Cell culture and RNA analysis Total RNA was extracted with QiaAmp RNA blood mini kit (Qiagen) from subconfluent keratinocytes of patients 38, 44, 62, 92 and 100, and a normal control cultivated in Keratinocyte Growth Medium (Invitrogen, Karlsruhe, Germany). Reverse transcription (RT) was performed with Advantage RT-for-PCR Kit (BD Biosciences, Heidelberg, Germany) with 0Æ5 lg of total RNA by using oligo dT primers. For RT-PCR of COL7A1 the following primers were used: F5: 5¢-CTGAGGAGCTGAAGCGAGTT-3¢ and R8: 5¢-GCTGTGGGCTGTGGTATTCT-3¢; F60: 5¢-CAGCAGGAGAAAAGGGTGAC-3¢ and R68: 5¢-CTGGGACACCAGGAAAACC-3¢, F89: 5¢-AGATGGTGCCAGTGGAAAAG-3¢ and R93: 5¢-GATCTCCCTTCACACCTGGA-3¢; F10: 5¢-TCCTTTCCTGGAACTTGGTG-3¢ and R27: 5¢-CAGACCACTGACTGCCTGGT-3¢; F102: 5¢-GGATGGTGACAAAGGACCTC-3¢ and R110: 5¢-GCAGAGCCATCATTTCCACT, respectively. PCR products were separated on 1Æ5% agarose gels, purified from the gel with the Qiagen gel purification kit and sequenced in both directions as described.9 Quantitative real-time polymerase chain reaction Quantitative real-time PCR and SYBR-Green I detection method was performed, as described.20,21 Primers for generation of small amplicons corresponding to COL7A1 exons 10–11, 11– 12, 13–14, 18–19 and 23–24 were designed. Amplicons corresponding to exon 4 (hsall 4F ⁄R) of the SALL4 gene were used as an internal reference. For real-time detection, the ABI Prism 7900 system and 384-well plates (both from PE Applied Biosystems, Norwalk, CT, U.S.A.) were used. Reactions contained 0Æ25 mmol L)1 of each primer and 5 lL of QuantiTect SYBR Green PCR Master Mix (Qiagen) in a final volume of 10 lL. Each run included samples of serially diluted control DNA (40 ng, 20 ng, 10 ng, 5 ng) for the generation of standard curves for each primer pair, and genomic DNA samples from patients, parents and controls (25 ng). The PCR programme consisted of 50 C for 2 min, 95 C for 15 min, and 40 cycles of 94 C for 15 s, 54 C ⁄60 C for 15 s, and 72 C for 1 min. To verify the specificity of the primers, melting curve analysis of the amplicons was performed and the results were evaluated as previously described.20 Analysis of the 1G 2G MMP1 gene polymorphism A rapid method for genotype analysis of the MMP1 gene 1G 2G polymorphism was employed as described.12,22 To verify the procedure, randomly selected samples were also sequenced 2009 The Authors Journal Compilation 2009 British Association of Dermatologists • British Journal of Dermatology 2009 161, pp1089–1097 Dystrophic epidermolysis bullosa and MMP1, J.S. Kern et al. 1091 using the primers: F 5¢-CCTCTGATGCCTCTGAGAAGA and R 5¢-TCCTCCCCTTATGGATTCCT for the PCR and sequencing reaction. In all cases, the results obtained by restriction enzyme digestion and sequencing were identical. Using SPSS software (Chicago, IL, U.S.A.), allele frequencies were analysed with Fisher’s exact test. Morphological analyses of the skin In most cases, the morphological diagnosis of DEB was ascertained with immunofluorescence mapping of blistered DEB skin using a panel of antibodies to components of the epidermal basement membrane zone or with transmission electron microscopy.23 Indirect immunofluorescence staining was performed as described and the sections were observed with an Axiophot fluorescence microscope (Carl Zeiss, Jena, Germany).9 Results The spectrum of dystrophic epidermolysis bullosa and disclosure of 42 novel COL7A1 mutations Our cohort consisted of 103 patients: 33 with dominant DEB (DDEB), 29 with RDEB-other (RDEB-O) and 41 with RDEBsevere generalized (RDEB-sev gen), as defined according to the revised epidermolysis bullosa classification (Tables S1 and S2; see Supporting information).1 Of the 103 patients, six had the clinical presentation of DEB pruriginosa (patients 1, 6, 14, 23, 25 and 37); in five cases the inheritance was dominant and in one recessive.24,25 Ten individuals with RDEB had one or several squamous cell carcinomas (patients 62, 63, 82, 87, 88, 89, 95, 96, 101, 102; Table S2; see Supporting information). As expected, mutations in patients with DDEB and RDEB-O resulted in the presence of low levels of collagen VII in the skin (Tables S1 and S2; see Supporting information). Mutation screening disclosed disease-causing mutations in 161 of the 163 expected mutated alleles. Forty-two novel mutations were identified, comprising 10 glycine substitutions, three missense mutations other than glycine substitutions, seven nonsense, 11 deletion ⁄insertion, and 11 splice site mutations (Table 1). The full mutation constellations of all individuals are described in Tables S1 and S2 (see Supporting information). These data demonstrate the high variability of mutations in DEB and contribute to the expanding COL7A1 mutation database. The first intragenic large deletion in COL7A1 In the case of patient 92, using genomic DNA for amplification, no PCR products were obtained for exons 13–24. These findings suggested the presence of a genomic deletion in a homozygous state in the region. This was confirmed by quantitative real-time PCR, which demonstrated in the patient a homozygous deletion, while in both parents the amount of genomic DNA in the investigated region was consistent with the status of heterozygous carrier of the deletion. To the best of our knowledge, this is the first intragenic large genomic deletion in COL7A1. The breakpoints have been identified and demonstrated that it spans over 4 kb starting in intron 12 and ending in exon 24; the deletion was designated as c.1637)240_3255del4064. A large deletion comprising 255– 520 kb encompassing nine to 15 genes including COL7A1 has been described before in a patient with moderately severe RDEB in compound heterozygous state with a splicing mutation.26 Novel splice site mutations The consequences of the novel splice site mutations were verified by mRNA studies and by predictions with the software NetGene2 (http://www.cbs.dtu.dk/services/NetPGene/) or FSPLICE (http://linux1.softberry.com) as shown in Table 2. Interestingly, three apparently silent mutations emerged as splice site mutations. In patient 44, sequencing of the entire coding sequence and exon ⁄intron boundaries of COL7A1 revealed no sequence changes, except one novel sequence variant, a homozygous transversion c.5499C>T in exon 64. This converts the codon GGC for glycine into a synonymous codon GGT at position 1833 (p.G1833G) (Fig. 1a). The splice site prediction performed with the software NetGene2 provided no evidence for modification of splicing. The software FSPLICE predicted that the mutation introduced a novel cryptic donor splice site in exon 64. RT-PCR with primers located in exons 60 (F) and 68 (R) disclosed in the patient’s sample a slightly lower band than the 426-bp band obtained in the control (Fig. 1b). One additional minor band was obtained in both the patient and the control. Sequencing demonstrated that the patient’s major band resulted from aberrant splicing of exon 64, which led to the deletion of 35 bp from the mRNA (designated on RNA level as r.5497_5532del). A novel cryptic donor splice site was activated at the site of the substitution )35 positions from the normal donor splice site (Fig. 1c). This is predicted to cause a frame shift starting with codon 1834, and formation of a premature termination codon, 25 codons downstream (p.E1834RfsX25). Both parents were heterozygous carriers of the mutation. The sequence variant was confirmed in the patient’s DNA sample and excluded from 100 control chromosomes by digestion with restriction enzyme MwoI (not shown). Two other apparent silent mutations, c.7017C>T, p.G2339G and c.7023G>A, p.K2341K, were predicted to interfere with the donor splice site of exon 90 (Fig. 1d,e). They did not completely abolish the normal splice site, but either created a novel donor splice site upstream (Fig. 1d), or activated a cryptic donor splice site downstream (Fig. 1e), respectively. In patient 62, the prediction regarding the mutation c.7023G>A was confirmed on the RNA level by RT-PCR. Presumably, in vivo, both normal and aberrant transcripts occur, resulting in RDEB-O in both patients. Finally, the consequences of the mutation c.7929+1G>A, which affects the conserved position +1 at the donor splice 2009 The Authors Journal Compilation 2009 British Association of Dermatologists • British Journal of Dermatology 2009 161, pp1089–1097 1092 Dystrophic epidermolysis bullosa and MMP1, J.S. Kern et al. No. Location exon ⁄ intron COL7A1 mutation cDNA Missense and nonsense mutations 1 22 2966G>A 2 32 3940G>A 3 60 5287C>T 4 66 5570G>A 5 73 6080C>T 6 73 6173G>C 7 74 6191G>T 8 75 6236G>T 9 78 6394G>A 10 84 6689G>A 11 85 6745C>T 12 88 6927G>C 13 96 7345G>A 14 101 7598G>A 15 102 7621C>T 16 103 7705G>A 17 108 7987G>T 18 111 8233C>T 19 112 8329C>T 20 117 8764C>T Splice site mutations 21 6 846G>A 22 6 846+1G>A 23 18 2441)2A>G 24 19 2587+1G>A 25 64 5499C>T 26 74 6217)3C>A 27 85 6751)2_1delAG 28 90 7017C>T 29 90 7023G>A 30 91 7068+5G>A 31 106 7929+1G>A Deletion ⁄ insertion mutations 32 13–24 1637)240_3255del4064 33 17 2305_2314delGTGAGGACTGinsTT 34 20 2638dupC 35 21 2789_2790dupAC 2791_2796del6 36 23 3020delC 37 27 3566delT 38 45 4590delA 39 78 6422delG 40 95 7289delC 41 105 7861_7865delCCCCG 42 111 8253_54dupAG Table 1 Novel COL7A1 mutations identified in this study Collagen VII protein ⁄ consequence Phenotype W989X G1314R R1763X G1857E P2027L G2058A G2064V G2079V G2132S G2230E Q2249X K2309N G2449R G2533D R2541X G2569S E2663X R2745X R2777X R2922C RDEB RDEB RDEB RDEB RDEB RDEB DDEB DDEB RDEB DDEB RDEB RDEB RDEB RDEB RDEB RDEB RDEB RDEB RDEB RDEB a RDEB RDEB RDEB RDEB RDEB RDEB RDEB RDEB RDEB RDEB RDEB a a a a a a a a a a PTC V769FfsX2 E880GfsX23 R931TfsX3 RDEB RDEB RDEB RDEB P1007QfsX9 M1189SfsX76 G1531EfsX177 G2141EfsX64 P2430QfsX35 P2621GfsX4 V2752EfsX34 RDEB RDEB RDEB RDEB RDEB RDEB RDEB RDEB, recessive dystrophic epidermolysis bullosa; DDEB, dominant dystrophic epidermolysis bullosa; PTC, premature termination codon. aSee Table 2. site of exon 106, were verified by RT-PCR. This demonstrated the presence of two transcripts: one resulted from skipping of exon 106 leading to an in-frame deletion of 18 codons, and the second resulted from inclusion of intron 106 into the reading frame leading to a frame shift and premature termination codon (PTC) (Fig. 1f). The 1G 2G MMP1 single nucleotide polymorphism in patients with dystropic epidermolysis bullosa and association with disease severity The 1G 2G MMP1 SNP genotype distribution was consistent with the Hardy–Weinberg equilibrium. The distribution of the 2009 The Authors Journal Compilation 2009 British Association of Dermatologists • British Journal of Dermatology 2009 161, pp1089–1097 Dystrophic epidermolysis bullosa and MMP1, J.S. Kern et al. 1093 Table 2 Splice site mutations discovered in this study and their consequences, as predicted by the splice-site predictor Splice-site scorea Location c.DNA position Normal Mutant Theoretical predictions at mRNA protein level Exon 6 ds)1 Intron 6 ds+1 Intron 18 as)2 Intron 19 ds+1 Exon 64 ds)34 Intron 74 as)3 Intron 85 as)2_1 Exon 90 ds)7 Exon 90 ds)1 846G>A 846+1G>A 2441)2A>G 2587+1G>A 5499C>T (p.G1833G) 6217)3C>A 6751)2delAG 7017C>T (p.G2339G) 7023G>A (p.K2341K) 0Æ88 0Æ88 5Æ40b 0Æ55 11c 0Æ98 1Æ00 1Æ00 1Æ00 LDS LDS LAS LDS 11 0Æ49 LAS 0Æ95 0Æ82 7068+5G>A 1Æ00 LDS 7929+1G>A 0Æ95 LDS Skip exon 6, FS, PTC Skip exon 6, FS, PTC, verified by RT-PCR Skip exon 18, IF Skip exon 19, IF Novel ds upstream, FS, PTC, verified by RT-PCR Skip exon 75, IF Skip exon 85, IF Novel ds upstream Activation of cryptic ds downstream, verified by RT-PCR, FS, PTC (i) Skip exon 91, IF (ii) Cryptic ds downstream (i) Skip exon 106, IF, verified by RT-PCR (ii) Inclusion of intron 106 into the mRNA, FS, verified by RT-PCR Intron 91 ds+5 Intron 106 ds+1 ds, donor splice site; as, acceptor splice site; LDS, loss of donor splice site; LAS, loss of acceptor splice site; FS, frame shift; PTC, premature termination codon; IF, in-frame; RT-PCR, reverse transcription–polymerase chain reaction. aIf not mentioned, predictions were made with NetGene2. bPredicted with FSPLICE, threshold 4Æ175. cPredicted with FSPLICE, threshold 6Æ099. (a) (c) (d) (e) (f) (b) Fig 1. Consequences of splice site mutations. (a) Direct sequencing of polymerase chain reaction (PCR) products from genomic DNA disclosed in patient 44 (upper panel) a novel homozygous transversion in exon 64: c.5499C>T which changed the codon GGC in the wild-type sequence to the synonymous codon GGT at position 1833, p.G1833G. This GT induced a new donor splice site (red circle in the upper panel). (b) In the upper panel, reverse transcription (RT)-PCR analysis with primers spanning exon 60–68 of COL7A1 demonstrated in patient 44 (P44) a transcript which was slightly smaller than the 426-bp transcript obtained in the control (Co). In the lower panel, RT-PCR with control primers for GAPDH is shown. One additional minor product was obtained in the patient and the control. (c) Sequencing demonstrated that the shorter major RT-PCR product in the patient resulted from aberrant splicing of exon 64 and skipping of the last 35 nucleotides of exon 64 (upper panel). The control sequence is shown in the lower panel. (d) Schematic representation of the predicted consequences of the mutation c.7017C>T resulting in a novel cryptic donor splice site (cds 1) in patient 53. The mutation (purple and bold) induced a new donor splice site (red circle) (NatGene2 score 1Æ00), while the score of the normal splice site downstream (green circle) decreased slightly from 1Æ00 to 0Æ95. Both splice sites might be active. (e) Schematic representation of the predicted consequences of the mutation c.7023G>A resulting in formation of a novel cryptic donor splice site (cds 2) in patient 62. The mutation (purple and bold) leads to the decrease of the score of the normal splice site (green circle) from 1Æ00 to 0Æ82, while the score of the cryptic splice site (red circle) located downstream increases from 0Æ7 to 0Æ9. Again, both donor splice sites might be active. (f) RT-PCR and sequencing (not shown) demonstrated the presence of two transcripts in patient 100 (P100) instead of the correct transcript obtained in the control sample (Co). The schematic representation shows that the abnormal transcripts resulted either from skipping of exon 106, or from inclusion of intron 106 in the mRNA. 2009 The Authors Journal Compilation 2009 British Association of Dermatologists • British Journal of Dermatology 2009 161, pp1089–1097 1094 Dystrophic epidermolysis bullosa and MMP1, J.S. Kern et al. 1G/1G EB DD 1G/2G en O B- E RD 2G/2G vg se B- E RD ls tro n Co Fig 2. Distribution of 1G ⁄ 1G, 1G ⁄ 2G and 2G ⁄ 2G genotypes in patients with dystrophic epidermolysis bullosa (DEB) and controls. The graph represents the percentage of patients and controls with 1G ⁄ 1G, 1G ⁄ 2G and 2G ⁄ 2G genotypes. DDEB, dominant DEB; RDEB-O, recessive DEB-other; RDEB-sev gen, recessive DEB-severe generalized. three genotypes 1G ⁄1G, 1G ⁄2G and 2G ⁄2G in patients and controls is shown in Figure 2 and Table 3. The major allele in our control group was 1G (52Æ5%), as reported in the NCBI SNP database for another control caucasian population (56Æ7%). The allelic frequency of 2G in DDEB (45Æ5%) was similar to our controls and to the NCBI control population mentioned above (47Æ5% and 43Æ3%). Notably, in the RDEBO and the RDEB-sev gen groups the major allele was 2G (58Æ6% and 52Æ4%), yet this increase, compared with controls, was not statistically significant (P = 0Æ23 and P = 0Æ64; Table 3). Interestingly, in the RDEB-O group, with all patients having residual collagen VII in the skin, the increased 2G frequency and therefore increased transcription of MMP1 could indeed play a role in degradation of the protein, and the status of this frequent SNP might play a role in the modulation of pathological processes in the skin. Next, we analysed possible associations of the 1G 2G MMP1 SNP with clinical phenotypes. We compared generalized and localized DDEB, and found no statistically significant difference in the 2G allele frequency. Therefore, in this cohort of patients with DDEB, the 1G 2G MMP1 SNP is not likely to act as a sole or strong disease modifier. We also compared the 1G 2G MMP1 SNP genotype of patients with RDEB-O and RDEB-sev gen harbouring mutations that allow residual expression of collagen VII. The RDEBsev gen cohort did not show a significant increase in 2G allele frequency, as compared with RDEB-O patients. In the group with clinical DEB pruriginosa, the 1G ⁄2G and 2G ⁄2G genotypes were found in five of six patients. Of 10 patients with RDEB who developed aggressive squamous cell carcinoma, four were homozygous 1G ⁄1G, three were heterozygous 1G ⁄2G and three were homozygous 2G ⁄2G. Thus, an increased association of the 2G allele was not found in this group of patients, and observations in this cohort differ from those reported by Almaani et al.19 MMP1 and disease severity in individual cases We further addressed the question of whether the 1G 2G MMP1 SNP could correlate with disease severity in individual situations. Four patients with RDEB-sev gen harboured COL7A1 mutations that allowed expression of collagen VII, in contrast to all others who had mutations leading to a PTC and complete absence of collagen VII in the skin. Patient 63 was compound heterozygous for a splice site (c.425A>G) and a missense (p.R2063W) mutation and was homozygous for the MMP1 SNP 2G allele. He had severe disease and died at the age of 34 years of aggressive squamous cell carcinoma. Patient 75 had a homozygous glycine substitution mutation p.G2449R and was heterozygous (1G ⁄2G) for the MMP1 SNP. He had an unexpectedly severe phenotype with mitten deformities. Predictions did not indicate any splicing abnormality. Immunofluorescence mapping revealed a reduced collagen VII signal at the dermal-epidermal junction. Patient 94 was homozygous for the mutation p.G1857E and for the MMP1 SNP 2G allele, and had severe blistering at birth, but had not yet developed severe scarring and mitten deformities, because of the young age (1 year). Immunofluorescence mapping indicated strong reduction of collagen VII at the dermal-epidermal junction. Predictions provided no evidence that the mutation Table 3 MMP1 single nucleotide polymorphism genotype and allele frequency Genotype DDEB RDEB-O RDEB-sev gen Controls CAUC1a 1G ⁄ 1G 1G ⁄ 2G 2G ⁄ 2G Total patient number 1G allele frequency 2G allele frequency 8 (24Æ2%) 20 (60Æ6%) 5 (15Æ2%) 33 54Æ5% 45Æ5% 1 (3Æ4%) 22 (75Æ9%) 6 (20Æ7%) 29 41Æ4% 58Æ6% 10 (24Æ4%) 19 (46Æ3%) 12 (29Æ3%) 41 47Æ6% 52Æ4% 6 (15%) 30 (75%) 4 (10%) 40 52Æ5% 47Æ5% 9 (30%) 16 (53Æ3%) 5 (16Æ7%) 30 56Æ7% 43Æ3% DDEB, dominant dystrophic epidermolysis bullosa; RDEB-O, recessive dystrophic epidermolysis bullosa-other; RDEB-sev gen, recessive dystrophic epidermolysis bullosa-severe generalized. aThirty individuals of caucasian heritage (http://www.ncbi.nlm.nih.gov/SNP/snp_ref. cgi?rs=1799750). 2009 The Authors Journal Compilation 2009 British Association of Dermatologists • British Journal of Dermatology 2009 161, pp1089–1097 Dystrophic epidermolysis bullosa and MMP1, J.S. Kern et al. 1095 In contrast, patient 85 had a severe phenotype comprising extensive chronic wounds, knee and elbow joint as well as hand contractures and webbing at the age of 9 years. Mucosal involvement led to severe oesophageal strictures, necessitating dilatation and placement of a percutaneous endoscopic gastrostomy tube, as well as to anal stenoses. He was compound heterozygous for the COL7A1 mutations p.[R1632X]+[E2059G] and homozygous for the 1G allele (Fig. 3a,b). In comparison, patient 34, the 56-year-old uncle of patient 85, homozygous for p.E2059G and homozygous 2G ⁄2G, was relatively mildly affected with RDEB-O (Fig. 3a,c). Collagen VII was decreased in the skin of both individuals (Fig. 3d–g). Therefore, in this constellation, it is likely that other disease modifiers account for the different phenotypes. (a) (c) (b) Discussion (d) (e) (f) (g) Fig 3. Clinical presentation and collagen VII expression in a family in which the clinical severity does not seem to correlate with the 1G 2G MMP1 single nucleotide polymorphism genotype. (a) Family pedigree showing patient 85 (nephew) and patient 34 (uncle) with recessive dystrophic epidermolysis bullosa and their COL7A1 and MMP1 genotypes. (b) Clinical presentation of the 9-year-old patient 85. The upper panel shows scarring and contractures of the fingers. The lower panel reveals extensive trauma-induced skin fragility of the back. (c) The 56-year-old uncle of patient 34 shows a much milder clinical appearance. The upper panel demonstrates atrophic scarring and mild finger contractures. In the lower panel, individual erythematous lesions on the skin of the back can be seen. (d–g) Indirect immunofluorescence staining of the skin with the collagen VII antibody LH7.2 demonstrates strong staining in control samples (d,f), and reduced, but positive signals in the skin of patients 85 (e) and 34 (g). The asterisk indicates the blister. could affect splicing. In all three cases, despite the presence of missense mutations, the increased transcription rate of MMP1 caused by the 2G allele present might contribute to the more severe phenotypes by degradation of residual anchoring fibrils. Identifying sources of disease variation is crucial to improving biologically valid therapeutic concepts for DEB. It is attractive to consider a genetic variant, which increases MMP1 expression, as a modulator of disease severity. However, given the relatively small numbers of patients available and the likely low magnitude of effect size, replication of results in independent populations is essential. Furthermore, mutation analysis and careful investigation of the consequences of mutations are essential in establishing genotype–phenotype correlations. Our results indicate that large genomic deletions and apparently silent mutations might account for a number of cases of DEB, and might be overlooked in a routine diagnostic procedure. Moreover, as COL7A1 mutation analysis is laborious, usually only the DNA of the index patient is analysed completely, and the mutations are then confirmed in related individuals. Therefore, within the same family the presence of other mutations or sequence variants explaining variability of phenotypes cannot be excluded. The results of the mutation analysis in our large cohort of 103 patients with DEB, disclosing 42 novel mutations, emphasizes the complexity of molecular mechanisms underlying DEB. Screening for COL7A1 mutations remains essential for understanding the pathogenesis of this devastating disease. In our cohort, patients with RDEB-O had an increased frequency of the 2G allele, but due to the limited number of cases no statistical significance was observed. In patients with RDEB-sev gen, the 2G allele might account for an increased severity in individual cases, as demonstrated by the examples of patients 63, 75 and 94, but it did not correlate with occurrence of squamous cell carcinoma. In the DDEB group we found no statistical association between the MMP1 genotypes and disease phenotype. In contrast to previously reported data, in our small group of patients with DEB pruriginosa, the genotypes 1G ⁄2G and 2G ⁄2G were predominant.19 These observations highlight the difficulty of obtaining sufficient statistical power to disclose real disease modifiers in rare diseases with relatively few affected individuals. Taken together, we cannot find clear-cut correlations between MMP1 promotor polymorphism and DEB phenotype 2009 The Authors Journal Compilation 2009 British Association of Dermatologists • British Journal of Dermatology 2009 161, pp1089–1097 1096 Dystrophic epidermolysis bullosa and MMP1, J.S. Kern et al. in our cohort of 103 patients. This question should be further addressed in a joint effort with as many patients with DEB as possible, to clarify the putative disease-modifying role of the MMP1 SNP. Moreover, measurement of the actual expression and activity of MMP1 in the skin of patients as well as the susceptibility of different mutated collagen VII variants to degradation would be necessary to confirm predicted effects. In vivo in the skin, the biological context is very complex and the individual contribution of a modifier gene, like MMP1 in this case, remains unknown. In cutaneous wounds in which the basement membrane is disrupted, as is the case with DEB, skin injury induces temporally and spatially restricted expression of MMP1 in migrating keratinocytes within hours.17 This expression is shut down after re-epithelialization is completed. MMP1 is also expressed in fibroblasts in granulation tissue, where it is believed to participate in remodelling of the ECM.17 The regulation of MMP1 activity depends not only on the expression levels, but also on activation of the proenzyme and on inhibition, mainly by TIMPs. These processes are finetuned to assure normal wound healing. In DEB, the basement membrane is repeatedly disrupted, and the chronic wound situation modifies the environment, leading to disturbances of the balance between proteases and inhibitors. Therefore, one might expect that a primary increase of MMP1 transcription would be compensated by other mechanisms to maintain tissue homeostasis, e.g. variation in the expression and activity of MMP activators and inhibitors, and that these might also be implicated in DEB severity. Future functional studies must clarify the partial roles of the 1G 2G MMP1 SNP and other modifying factors in the complex interplay of cell–matrix interactions in healing DEB skin. Other modifier genes are certainly involved in modulation of phenotypic variations in different forms of epidermolysis bullosa.27 For example, the splicing machinery is known to be a genetic modifier in single-gene disorders. Patients with splicing mutations can have variations in the level of correctly spliced RNA transcribed, which correlates with the disease severity.28 In the case of missense mutations, mutant proteins can be misfolded and subjected to intracellular degradation, processes which are likely to be the subject of interindividual genetic variations.29 New approaches such as genetic modifier screens in model organisms or biodata mining will help identify novel candidates for disease modifiers in the future.30,31 Acknowledgments We thank all patients who participated in this study, the physicians who sent us samples and Martin Festag for help with RNA-analysis. The work was supported by a Network Epidermolysis Bullosa grant from the Federal Ministry for Education and Research to L.B.-T. and by the Excellence Initiative of the German Federal and State Governments (Spemann Graduate School of Biology and Medicine to J.S.K., and Freiburg Institute for Advanced Studies, School of Life Sciences to L.B.-T.). References 1 Fine JD, Eady RA, Bauer EA et al. The classification of inherited epidermolysis bullosa (EB): Report of the Third International Consensus Meeting on Diagnosis and Classification of EB. J Am Acad Dermatol 2008; 58:931–50. 2 Kern JS, Has C. Update on diagnosis and therapy of inherited epidermolysis bullosa. Expert Rev Dermatol 2008; 3:721–33. 3 Varki R, Sadowski S, Uitto J et al. Epidermolysis bullosa. II. Type VII collagen mutations and phenotype–genotype correlations in the dystrophic subtypes. J Med Genet 2007; 44:181–92. 4 Aumailley M, Has C, Tunggal L et al. Molecular basis of inherited skin-blistering disorders, and therapeutic implications. Expert Rev Mol Med 2006; 8:1–21. 5 Has C, Bruckner-Tuderman L. Molecular and diagnostic aspects of genetic skin fragility. J Dermatol Sci 2006; 44:129–44. 6 Wessagowit V, Kim SC, Woong Oh S, McGrath JA. Genotype– phenotype correlation in recessive dystrophic epidermolysis bullosa: when missense doesn’t make sense. J Invest Dermatol 2005; 124:863–6. 7 Gardella R, Castiglia D, Posteraro P et al. Genotype–phenotype correlation in Italian patients with dystrophic epidermolysis bullosa. J Invest Dermatol 2002; 119:1456–62. 8 Shimizu H, McGrath JA, Christiano AM et al. Molecular basis of recessive dystrophic epidermolysis bullosa: genotype ⁄ phenotype correlation in a case of moderate clinical severity. J Invest Dermatol 1996; 106:119–24. 9 Kern JS, Kohlhase J, Bruckner-Tuderman L et al. Expanding the COL7A1 mutation database: novel and recurrent mutations and unusual genotype–phenotype constellations in 41 patients with dystrophic epidermolysis bullosa. J Invest Dermatol 2006; 126:1006– 12. 10 Dang N, Murrell DF. Mutation analysis and characterization of COL7A1 mutations in dystrophic epidermolysis bullosa. Exp Dermatol 2008; 17:553–68. 11 Bruckner-Tuderman L. Secondary modifiers and the phenotypic variability of junctional epidermolysis bullosa. Acta Derm Venereol (Stockh) 2008; 88:436. 12 Titeux M, Pendaries V, Tonasso L et al. A frequent functional SNP in the MMP1 promoter is associated with higher disease severity in recessive dystrophic epidermolysis bullosa. Hum Mutat 2008; 29:267–76. 13 Reynolds JJ. Collagenases and tissue inhibitors of metalloproteinases: a functional balance in tissue degradation. Oral Dis 1996; 2:70– 6. 14 Bauer EA, Gedde-Dahl T Jr, Eisen AZ. The role of human skin collagenase in epidermolysis bullosa. J Invest Dermatol 1977; 68:119– 24. 15 Stricklin GP, Welgus HG, Bauer EA. Human skin collagenase in recessive dystrophic epidermolysis bullosa. Purification of a mutant enzyme from fibroblast cultures. J Clin Invest 1982; 69:1373–83. 16 Bodemer C, Tchen SI, Ghomrasseni S et al. Skin expression of metalloproteinases and tissue inhibitor of metalloproteinases in sibling patients with recessive dystrophic epidermolysis and intrafamilial phenotypic variation. J Invest Dermatol 2003; 121:273–9. 17 Toriseva M, Kahari VM. Proteinases in cutaneous wound healing. Cell Mol Life Sci 2009; 66:203–24. 18 Rutter JL, Mitchell TI, Buttice G et al. A single nucleotide polymorphism in the matrix metalloproteinase-1 promoter creates an Ets binding site and augments transcription. Cancer Res 1998; 58:5321– 5. 19 Almaani N, Liu L, Harrison N et al. New glycine substitution mutations in type VII collagen underlying epidermolysis bullosa pruriginosa but the phenotype is not explained by a common 2009 The Authors Journal Compilation 2009 British Association of Dermatologists • British Journal of Dermatology 2009 161, pp1089–1097 Dystrophic epidermolysis bullosa and MMP1, J.S. Kern et al. 1097 20 21 22 23 24 25 26 27 polymorphism in the matrix metalloproteinase-1 gene promoter. Acta Derm Venereol (Stockh) 2009; 89:6–11. Borozdin W, Boehm D, Leipoldt M et al. SALL4 deletions are a common cause of Okihiro and acro–renal–ocular syndromes and confirm haploinsufficiency as the pathogenic mechanism. J Med Genet 2004; 41:e113. Has C, Wessagowit V, Pascucci M et al. Molecular basis of Kindler syndrome in Italy: novel and recurrent Alu ⁄ Alu recombination, splice site, nonsense, and frameshift mutations in the KIND1 gene. J Invest Dermatol 2006; 126:1776–83. Dunleavey L, Beyzade S, Ye S. Rapid genotype analysis of the matrix metalloproteinase-1 gene 1G ⁄ 2G polymorphism that is associated with risk of cancer. Matrix Biol 2000; 19:175–7. Bruckner-Tuderman L, Hopfner B, Hammami-Hauasli N. Biology of anchoring fibrils: lessons from dystrophic epidermolysis bullosa. Matrix Biol 1999; 18:43–54. Schumann H, Has C, Kohlhase J et al. Dystrophic epidermolysis bullosa pruriginosa is not associated with frequent FLG gene mutations. Br J Dermatol 2008; 159:464–9. Broekaert SM, Knauss-Scherwitz E, Biedermann T et al. Epidermolysis bullosa pruriginosa due to a glycine substitution mutation in the COL7A1-gene. Acta Derm Venereol (Stockh) 2006; 86:556–7. Titeux M, Mejia JE, Mejlumian L et al. Recessive dystrophic epidermolysis bullosa caused by COL7A1 hemizygosity and a missense mutation with complex effects on splicing. Hum Mutat 2006; 27:291–2. Dang N, Klingberg S, Rubin AI et al. Differential expression of pyloric atresia in junctional epidermolysis bullosa with ITGB4 mutations suggests that pyloric atresia is due to factors other than the mutations and not predictive of a poor outcome: three novel 28 29 30 31 mutations and a review of the literature. Acta Derm Venereol (Stockh) 2008; 88:438–48. Nissim-Rafinia M, Kerem B. The splicing machinery is a genetic modifier of disease severity. Trends Genet 2005; 21:480–3. Bateman JF, Boot-Handford RP, Lamande SR. Genetic diseases of connective tissues: cellular and extracellular effects of ECM mutations. Nat Rev Genet 2009; 10:173–83. Kucherenko MM, Pantoja M, Yatsenko AS et al. Genetic modifier screens reveal new components that interact with the Drosophila dystroglycan–dystrophin complex. PLoS ONE 2008; 3:e2418. Reverter A, Ingham A, Dalrymple BP. Mining tissue specificity, gene connectivity and disease association to reveal a set of genes that modify the action of disease causing genes. BioData Min 2008; 1:8. Supporting information Additional Supporting information may be found in the online version of this article: Table S1 COL7A1 mutations and MMP1 genotypes in patients with dominant dystrophic epidermolysis bullosa Table S2 COL7A1 mutations and MMP1 genotypes in patients with recessive dystrophic epidermolysis bullosa Please note: Wiley-Blackwell are not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article. 2009 The Authors Journal Compilation 2009 British Association of Dermatologists • British Journal of Dermatology 2009 161, pp1089–1097